Disease Spread

How does climate change contribute to the spread of infectious diseases ?
Climate change contributes to the spread of infectious diseases by increasing temperature and humidity, altering vector habitats, causing extreme weather events, and promoting urbanization and deforestation. These factors create favorable conditions for pathogens and disease vectors, disrupt sanitation systems, increase human-wildlife contact, and facilitate rapid disease spread among humans. Addressing these issues requires a comprehensive approach that includes mitigating climate change and implementing effective public health strategies.

Can asymptomatic individuals spread COVID-19 ?
Asymptomatic individuals can spread COVID-19, making preventive measures crucial.

How does climate change affect the spread of vector-borne diseases like dengue and malaria ?
Climate change has a significant impact on the spread of vector-borne diseases like dengue and malaria. The increased temperatures, changes in precipitation patterns, urbanization, deforestation, global travel, and trade all contribute to the spread of these diseases. Warmer temperatures can lead to an increase in the number of breeding sites for mosquitoes, while heavy rainfall can create temporary pools of standing water that serve as ideal breeding grounds for mosquitoes. Urbanization leads to denser human populations living in close proximity to each other, making it easier for mosquitoes to find hosts and spread diseases. Deforestation disrupts ecosystems and removes natural barriers that limit the spread of mosquitoes. Global travel allows people to carry diseases across borders, introducing new strains of viruses into areas where they were previously absent. Trade in goods and products can introduce new species of mosquitoes into areas where they were not previously found. By understanding how climate change affects these diseases, we can take steps to mitigate its effects and protect public health.

How does social distancing help prevent the spread of COVID-19 ?
Social distancing is a crucial measure in preventing the spread of COVID-19 by reducing contact with infected individuals, slowing down the virus's spread, decreasing case numbers, and flattening the curve.

What role does anthropogenic activity play in the emergence and spread of viruses ?
This text discusses the role of human activities in the emergence and spread of viruses, highlighting deforestation, urbanization, agricultural practices, and global travel as significant contributors. It suggests actions to mitigate these effects, such as protecting natural habitats and promoting sustainable agriculture, and emphasizes the need for improved public health infrastructure and responsible travel practices.
How do scientists use epidemiological data to trace virus origins ?
Epidemiology is the study of how diseases spread among populations. When a new virus emerges, scientists use epidemiological data to trace its origins. This involves several steps: collection of data about the disease, analysis of data to identify patterns, genomic sequencing to determine the relationship between viruses, field investigations to gather more information, and collaboration with other scientists to build a comprehensive picture of the virus's origins. By understanding how a virus emerged and spread, scientists can develop better strategies for preventing and controlling future outbreaks.
How does climate change influence the distribution and survival of disease-carrying organisms ?
This text discusses the influence of climate change on the distribution and survival of disease-carrying organisms, highlighting how altered habitats, changes in reproduction and life cycle, and altered behavior and transmission rates contribute to the spread of diseases. It further provides examples of specific disease-carrying organisms affected by climate change and suggests mitigation strategies such as surveillance, control measures, public health education, and research to address these challenges.

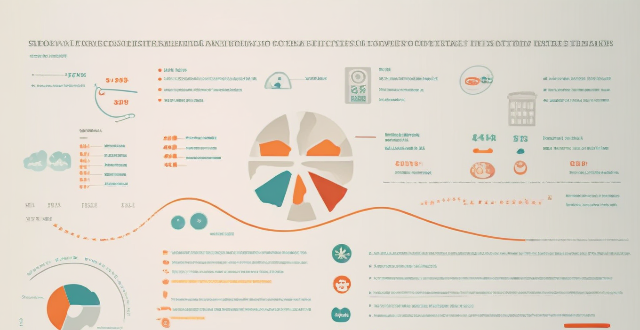
How does predictive analytics help in disease prevention and management within the healthcare system ?
Predictive analytics in healthcare can significantly improve disease prevention and management by identifying patterns and trends in patient data. It offers benefits such as early intervention, personalized treatment plans, enhanced operational efficiency, and informed decision-making. Applications include disease surveillance, chronic disease management, and patient care optimization. However, challenges like data privacy, quality, and the need for skilled data analysts must be addressed to fully realize its potential.

How does proper handwashing technique prevent the spread of germs ?
Proper handwashing is a simple yet effective way to prevent the spread of germs. It involves using soap and water to clean your hands thoroughly, especially before eating or preparing food, after using the restroom, and after being in contact with someone who is sick. The key points on how proper handwashing technique can help prevent the spread of germs include: - Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap. - Lather your hands by rubbing them together with the soap. Be sure to lather the backs of your hands, between your fingers, and under your nails. - Scrub your hands for at least 20 seconds. Need a timer? Hum the "Happy Birthday" song from beginning to end twice. - Rinse your hands well under clean, running water. - Dry your hands using a clean towel or air dry them. By following these steps, you can effectively remove dirt, viruses, and bacteria from your hands, which can help prevent the spread of germs that cause infections like the common cold and flu. Additionally, proper handwashing technique can also help prevent the spread of more serious illnesses such as COVID-19, Ebola, and norovirus.

Can exercise reverse heart disease ?
Heart disease is a major cause of death worldwide, and it can be devastating to those affected. While there are many treatments available for heart disease, including medication and surgery, some people wonder if exercise can reverse the damage caused by heart disease. There is evidence that regular exercise can help prevent and manage heart disease by improving cardiovascular health, managing weight, lowering blood pressure, improving cholesterol levels, and reducing stress. However, there is no conclusive evidence that exercise can completely reverse heart disease. Despite this, there are still many benefits to regular exercise for heart health. If you have been diagnosed with heart disease or are at high risk for developing it, talk to your doctor about starting an exercise program. They can help you create an exercise plan that is safe and effective for your individual needs and goals.

Is social distancing a long-term solution for controlling the spread of viruses ?
Social distancing is an effective measure for controlling the spread of viruses in the short term, but its feasibility as a long-term solution depends on various factors such as the nature of the virus, availability of medical resources, and willingness of people to adhere to guidelines. Other measures such as mask-wearing, hand hygiene, contact tracing, regular testing, and vaccine development should also be considered alongside social distancing to effectively control the spread of viruses over time.
What strategies have been successful in controlling the spread of COVID-19 in other countries ?
Successful strategies in controlling the spread of COVID-19 include early detection and response through testing and contact tracing, stringent lockdown measures, public health campaigns and education, and investment in healthcare infrastructure. Examples of countries that have implemented these strategies effectively include South Korea, New Zealand, Italy, India, Singapore, Germany, and Canada. By learning from these examples, other countries can improve their own responses to the pandemic and work towards containing its spread.

How effective are cloth masks compared to surgical masks in preventing the spread of COVID-19 ?
This article discusses the effectiveness of cloth masks compared to surgical masks in preventing the spread of COVID-19. Cloth masks are washable, reusable, and customizable, but they do not have the same level of filtration as surgical masks. Surgical masks are disposable, have a high filtration efficiency, and are designed for use by healthcare professionals during medical procedures. The choice between cloth masks and surgical masks depends on personal preference, availability, and specific circumstances. It is essential to follow guidelines from health organizations and authorities regarding the use of masks to help prevent the spread of COVID-19.

How do vaccines work to protect against disease ?
Vaccines protect against disease by introducing a small amount of the pathogen into the body, triggering the immune system to produce antibodies that protect against future infections with the same pathogen. There are several types of vaccines with unique mechanisms of action and effectiveness against specific pathogens. The development of vaccines is a complex process requiring extensive testing and research, but they have been shown to be highly effective at preventing serious diseases.

What are some good gluten-free food options for people with celiac disease ?
Celiac disease is an autoimmune disorder that damages the small intestine and requires a strict gluten-free diet. Good gluten-free food options for people with celiac disease include fruits and vegetables, meat and fish, gluten-free grains and starches like quinoa and brown rice, dairy products, nuts and seeds, gluten-free flours and baking mixes, and gluten-free snacks and beverages like popcorn and juices.
What measures can be taken to prevent the spread of infectious diseases across borders ?
The text discusses measures to prevent the spread of infectious diseases across borders, including surveillance and early warning systems, travel restrictions and border controls, vaccination programs, public health infrastructure and preparedness, collaboration and information sharing, and education and public awareness. The Global Health Security Agenda (GHSA) promotes robust surveillance systems for early detection of outbreaks, while the International Health Regulations (IHR) require countries to develop core public health capacities. Travel restrictions such as entry/exit screening and quarantine policies can help prevent introduction of diseases into new regions. Vaccination programs, including routine immunization and vaccination requirements for travelers, reduce the risk of disease spread. Strong public health infrastructure and emergency response plans are crucial for containing outbreaks. Collaboration and information sharing through global health security initiatives and open access to data enable quicker identification of patterns and trends. Education and public awareness campaigns can reduce transmission rates and discourage travel to high-risk areas. By implementing these measures, countries can work together to protect public health globally.

How can we prevent the spread of virus variants ?
To prevent the spread of virus variants, a multifaceted approach is necessary, including vaccination, regular testing and isolation, public health measures such as mask-wearing and physical distancing, travel restrictions and quarantine, research and surveillance, and community action. Staying up-to-date with boosters and improving indoor ventilation can also help maintain protection against new variants.
What are the potential health risks associated with global warming ?
Global warming, caused by human activities, poses various health risks including heat-related illnesses like heatstroke and dehydration, spread of diseases such as malaria and Lyme disease, respiratory problems including asthma and allergies, and mental health issues like anxiety, depression, and PTSD. It is crucial to take measures to mitigate these effects and safeguard public health.

What are the key challenges facing global health security today ?
Global health security faces several key challenges, including emerging infectious diseases, antimicrobial resistance, weak health systems, political instability and conflict, and social determinants of health. These challenges threaten the well-being of people worldwide and require collective efforts to prevent, detect, and respond to infectious diseases that threaten human health.

What is the impact of virus variants on public health ?
Virus variants are mutations that occur in viruses, which can affect their ability to cause disease. These mutations can be beneficial or harmful to public health depending on the virus and its characteristics. The essay explores the impact of virus variants on public health and discusses some of the key factors that influence their spread and severity. The importance of virus variants is highlighted as they can change the way a virus spreads and affects people. For example, the SARS-CoV-2 virus has several variants, including the Omicron variant, which is more transmissible than previous versions. This means that it can spread more easily from person to person, leading to higher rates of infection and hospitalization. Virus variants can also affect the effectiveness of vaccines and treatments. Vaccines are designed to target specific strains of a virus, but if a new variant emerges, it may not be as effective at preventing infection or reducing symptoms. Similarly, treatments may not work as well against certain variants, making them less effective at treating infections. Factors that influence virus variants include mutation rate, population density, and environmental factors. High mutation rates make it difficult for scientists to predict how viruses will behave over time and create challenges for public health officials when trying to control outbreaks. Population density increases the likelihood that new variants will emerge and spread rapidly through a population. Environmental factors such as temperature and humidity can affect how viruses survive outside of humans and how they spread inside of them. In conclusion, virus variants can have a significant impact on public health by changing how viruses spread and affecting the effectiveness of vaccines and treatments. Understanding the factors that influence virus variants is crucial for developing strategies to prevent and control outbreaks. As we continue to learn more about these viruses, it is important to stay informed and take steps to protect ourselves and others from infection.

Does high-intensity interval training (HIIT) have specific benefits for chronic disease prevention ?
High-intensity interval training (HIIT) offers numerous benefits for chronic disease prevention, including improved cardiovascular health, enhanced glucose control, reduced inflammation, increased muscle mass and strength, and improved mental health outcomes. To incorporate HIIT into a healthy lifestyle, start slowly, choose the right exercises, include other forms of exercise, and consult with a health professional.
How much exercise is needed per week to prevent chronic disease ?
Chronic diseases are a major cause of death and disability worldwide. Regular physical activity can help reduce the risk of developing chronic diseases such as heart disease, diabetes, and some types of cancer. According to the World Health Organization (WHO), adults should aim to do at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise each week, along with muscle-strengthening activities at least twice a week. However, the amount of exercise needed to prevent chronic diseases may vary depending on individual factors such as age, sex, body weight, and overall health status. It's recommended that people try to incorporate at least 30 minutes of moderate-intensity aerobic exercise into their daily routine, along with strength training exercises whenever possible.
How does consistent physical activity affect the immune system in relation to chronic disease prevention ?
The article discusses the impact of consistent physical activity on the immune system and its role in preventing chronic diseases. It explains that regular exercise can increase the number and activity of immune cells, reduce inflammation, and improve overall health. The article also provides recommendations for exercise and emphasizes the importance of incorporating physical activity into one's lifestyle to prevent chronic diseases and improve well-being.

Can studying animal populations help us understand virus origins ?
Viruses often originate from animals, making the study of animal populations crucial for understanding virus origins and preventing disease outbreaks. Zoonotic diseases like influenza, HIV, and Ebola highlight the connection between animal and human health. Identifying animal reservoirs and understanding spillover mechanisms are key to preventing virus transmission. The "One Health" approach emphasizes collaboration across disciplines to address health risks at the human-animal-ecosystem interface. Conservation efforts and maintaining ecosystem health can reduce the risk of zoonotic diseases by preserving biodiversity and minimizing human-wildlife contact. Overall, monitoring animal populations is essential for anticipating and mitigating viral disease emergence and spread.

What are the potential impacts of climate change on different sectors ?
Climate change affects various sectors differently. In agriculture, changes in crop yields, shifts in planting seasons, increased pest and disease pressure, and water scarcity may occur. Health issues include heat-related illnesses, spread of diseases, air quality problems, and mental health concerns. Economic impacts involve job losses, infrastructure damage, supply chain disruptions, and investment risks. Environmental effects encompass loss of biodiversity, ocean acidification, deforestation, and sea level rise. It is crucial for all stakeholders to take measures to mitigate these impacts and adapt to the changing climate.